NSQHS Mandatory Compliance for Dental Infection control systems
In January 2013, the National Safety and Quality Health Service (NSQHS) came into effect requiring mandatory compliance for all public and private hospital and day surgeries and the majority of public dental practices.
For private dental practices however, accreditation to the NSQHS Standards is voluntary. The Australian Dental Association provides support for private practices who wish to participate in the scheme.
In November 2015 the Australian Commission on Safety and Quality in Health Care released a guide for Dental practices and services.
So what does this mean for dental surgeries and what do they need to do to comply with regard to infection control?
The NSQHS standard is made up of 10 individual standard documents but dental practices only need to be accredited to NSQHS standards 1-6 as standards 7-10 are not relevant in the dental care setting.
Six Standards for Dental Practices
The six standards for Dental practices are:
- Governance for Safety and Quality in Health Service Organisations
- Partnering with Consumers
- Preventing and Controlling Healthcare Associated Infections
- Medication Safety
- Patient Identification and Procedure Matching
- Clinical Handover
Each standard has a number of core actions (mandatory) and development actions (non-mandatory but recommended). The standard relating to infection control is Standard 3 - Preventing and Controlling Healthcare Associated Infections.
‘The intention of this Standard is to minimise the risk for patients in acquiring preventable infections and to use evidence-based strategies to effectively manage infections when they occur.’
Standard 3 consists of six criteria:
- Governance and systems for infection prevention, control and surveillance – you must have integrated systems of governance in place to manage patient safety and quality risks.
- Infection prevention and control strategies – you must develop, implement and maintain strategies for the prevention and control of healthcare associated infections.
- Managing patients with infections or colonisations – you must have systems in place that are able to promptly identify patients who acquire an infection during their care.
- Antimicrobial stewardship – you must implement a system of antimicrobial stewardship. The inappropriate use of antimicrobials can increase the risk of resistant bacteria.
- Cleaning, disinfection and sterilisation – you must implement a system that meets current best practices and standards.
- Communicating with patients and carers - a system must be established to provide information to patients regarding healthcare associated infections.
You need to implement, policies, procedures and protocols that comply with the National Health and Medical Research council - Australian Guidelines for the Prevention and Control of Infection in Health Care, The National Hand Hygiene initiative, Australian Immunisation Handbook, Antimicrobial stewardship program, Therapeutic Guidelines: Antibiotic, Therapeutic Guidelines: Oral and Dental.
Dental Board of Australia’s Guidelines for Infection Control.
The Dental Board of Australia’s Guidelines for Infection Control states that ‘every place where dental care is provided must have the following documents:
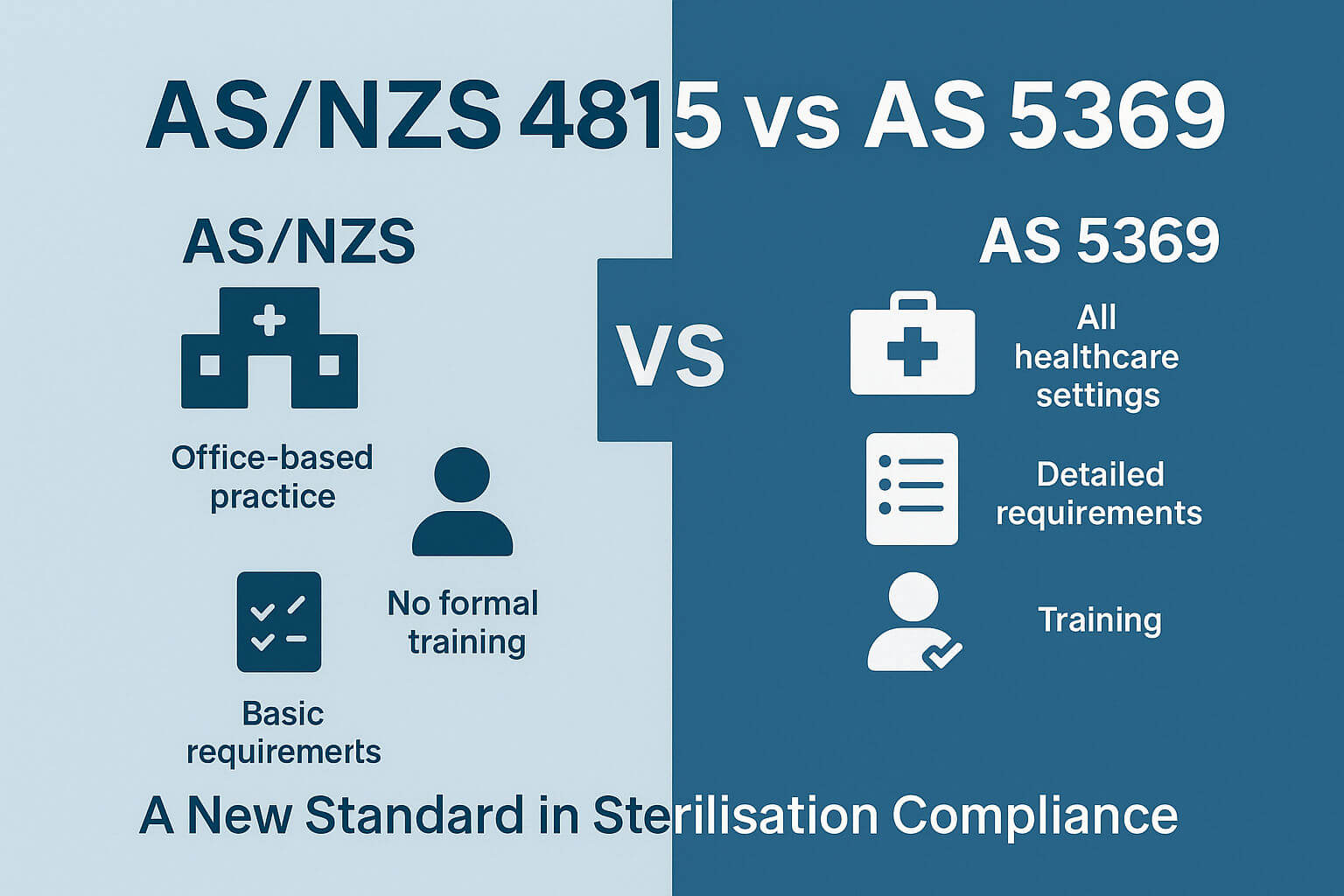
A manual setting out the infection control protocols, AS/NZS 4815 or AS/NZS 4187, Australian Guidelines for the Prevention and Control of Infection in Health Care, Australian Dental Association Guidelines for infection Control.
Specifically, Section 3.16 of the NSQHS standard states:
‘You should ensure that the policies, procedures or protocols for cleaning, disinfection and sterilisation of reusable instruments and devices are aligned with current national or international standards.’
Given the Dentals Boards guidelines, you could probably safely assume that this would mean adherence to AS4815 or AS4187 depending on the size of your clinic. However, the NSQHS does have some specific requirements as well.
There is a requirement to implement a system of traceability that enables individual identification of patients and the reusable instruments and devices used.
It’s clear from this that you need to track sterilized items to their use on patients. The standard goes further to specify, ‘especially critical items used on patients during dental procedures’. You could take that to mean that all items; critical, semi critical and non-critical (see this blog) need to be tracked to patients.
It goes further to say that details of the instrument batches (sterilizing cycles) should be included in the patient’s dental record.
You should have (at the very least) a system in place of batch code identification, which refer back to the sterilization cycle records which may include:
- batch numbers
- individual items or sets of items
- patients on whom the items are used
- dates
- steriliser identification
- cycles
- operators responsible for release of the item for use
- Sterile stock from external providers.
Check out our new guide:
Conclusion
There is obviously a lot that needs to be done to comply with NSQHS, and tracking surgical instruments is a critical component of that. There are a number of ways you could go about that from a modern automated tracking system to stickers and guns to pen and paper.
There are a number of very useful clinical scenarios on page 103 and 104 of the NSQHS guide for Dental services that could assist you in working out the best way to go for you.
Using AS4815 and AS4187 as the platform to base your NSQHS compliance on should give you a head start.