TGA vs AS 5369: Closing the Gap in Surgical Traceability

Introduction
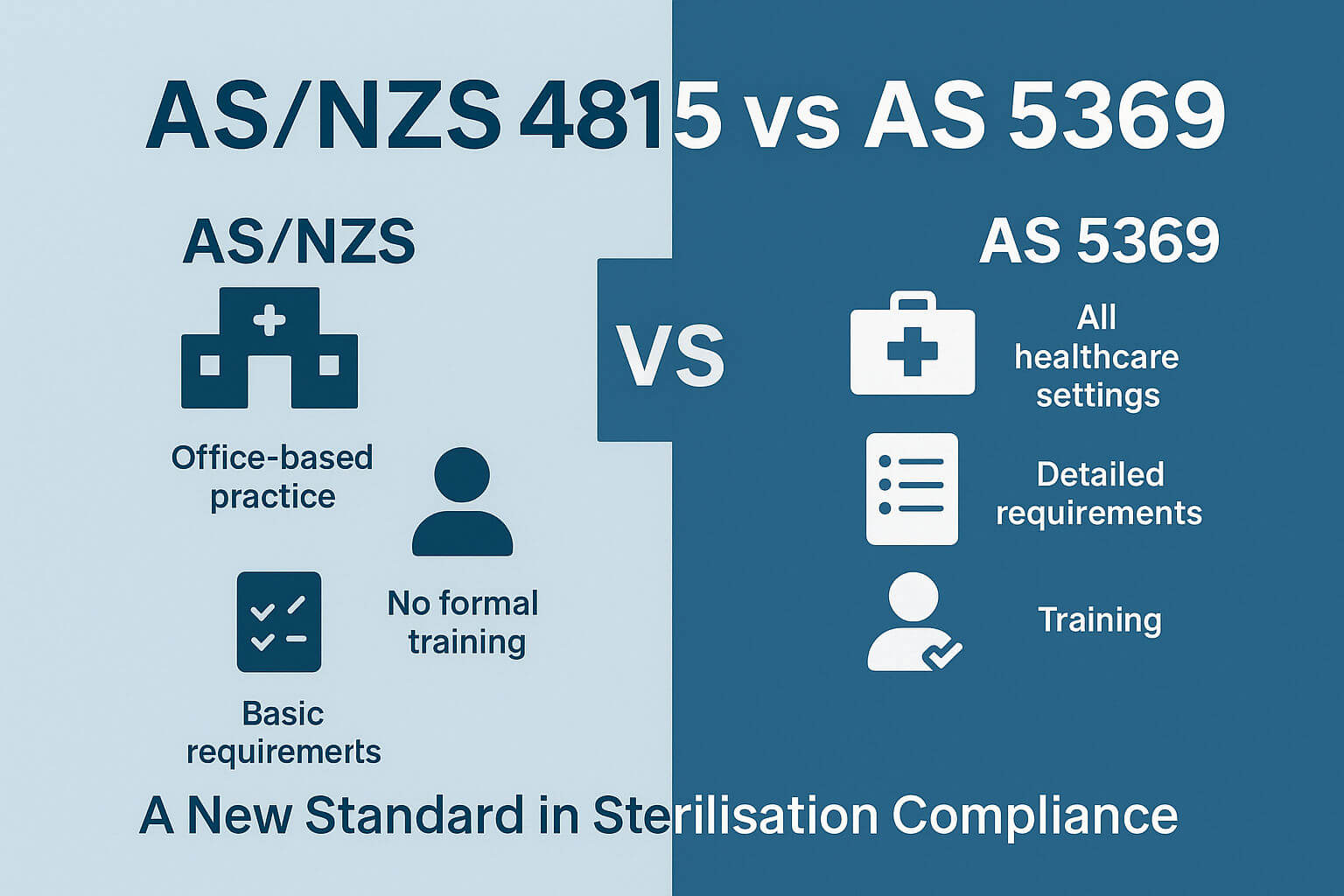
In the modern healthcare environment, where safety, traceability, and compliance are paramount, Australia’s regulatory framework for reusable surgical instruments presents a perplexing disconnect. On one hand, the recently published AS 5369:2023 sets a clear expectation for tracking surgical instruments from sterilization through to patient use. On the other, the Therapeutic Goods Administration (TGA) — Australia's national regulator — does not currently require direct part marking or Unique Device Identification (UDI) for Class I reusable surgical instruments, which make up the bulk of surgical tools used in clinical practice.
This divergence between clinical best practice and regulatory requirements is more than just an academic discrepancy — it has real-world implications for patient safety, operational efficiency, and the traceability of critical medical assets. In this article, we explore the current landscape, compare global standards, and ask whether the TGA is overdue for an update.
The Role of AS 5369:2023 in Reprocessing Traceability
Published as the new Australian standard for reprocessing reusable medical devices in health and non-health settings, AS 5369:2023 builds on the foundation of best practice established in previous sterilization guidelines. A major emphasis of this standard is instrument traceability — not only through reprocessing workflows but all the way to point-of-use on the patient.
Specifically, AS 5369 calls for:
-
Full traceability of critical and semi-critical instruments
-
The use of electronic or manual tracking systems
-
Recording of patient ID, sterilization cycle, and device usage
-
Support for unique identification of instruments, where possible
This is in line with international best practices and reflects increasing concerns about infection control, surgical site infections, and quality assurance across Australian health services.
UDI: The Global Push for Device Identification
The Unique Device Identification (UDI) system is a cornerstone of modern medical device traceability. It enables:
-
Efficient recalls and adverse event investigations
-
Improved inventory and reprocessing control
-
Assurance that devices used on patients are properly sterilized and traceable
UDI generally includes two components:
-
Device Identifier (DI): A static code representing the manufacturer and device model.
-
Production Identifier (PI): Dynamic data such as serial number, batch/lot, or expiry date.
Comparing the TGA, FDA, and EU Regulations
| Regulator | UDI on Reusable Surgical Instruments | Direct Part Marking | Class I Devices Covered? | PI Required in Database? |
|---|---|---|---|---|
| FDA (USA) | ✅ Yes | ✅ Yes (21 CFR 801.45) | ✅ Yes | ✅ Yes |
| EU MDR | ✅ Yes (Article 18) | ✅ Yes | ✅ Yes | ❌ No (PI on label only) |
| TGA (Australia) | ❌ Not yet required | ❌ No | ❌ No | ❌ No |
Both the FDA and EU MDR mandate UDI for all device classes, including Class I reusable surgical instruments, and enforce direct marking on instruments that are reprocessed and reused. These requirements support high traceability and patient safety.
By contrast, the TGA's phased UDI rollout focuses initially on Class III, AIMDs, and Class IIb/IIa devices, while Class I instruments — including most reusable surgical tools — are currently exempt.
Why the Gap Matters
This regulatory lag creates significant challenges:
-
Contradicts Clinical Guidelines
AS 5369 recommends unique identification for instruments to fulfill traceability requirements. But without a regulatory driver like UDI, uptake across all facilities is inconsistent. -
Undermines National Consistency
Hospitals and sterilization units may implement their own systems (e.g., laser-engraved barcodes), but without a standardised approach, interoperability and data aggregation become difficult. -
Hampers Recall and Incident Response
If a surgical instrument model is found to be defective or improperly sterilized, tracking its usage across patients becomes harder without a direct identifier or national database entry. -
Adds Administrative Burden
Facilities may resort to manual logs or homegrown databases, increasing the risk of error and inefficiency.
The Case for Direct Part Marking in Class I Instruments
Even though Class I reusable instruments are considered low-risk, they often:
-
Penetrate the skin and open body cavities
-
Come into contact with blood and tissue
-
Are used in multiple procedures across patients
-
Require rigorous cleaning, disinfection, and sterilization
This places them squarely within the domain of devices that should be traceable to support infection control and patient safety. Implementing direct part marking — such as laser-engraved GS1 DataMatrix codes — would be a relatively low-cost, high-benefit solution that aligns regulatory compliance with clinical realities.
What’s Holding the TGA Back?
The TGA’s current stance is shaped by several factors:
-
Focus on higher-risk devices during initial UDI rollout
-
Desire to minimise burden on manufacturers of Class I devices
-
Lack of immediate national-level enforcement for AS 5369 recommendations
But this should not delay future alignment. In fact, the groundwork laid by the Australian UDI Database (AusUDID) and the principles of AS 5369 make a strong case for expanding the scope of UDI in the next phase of reform.
Preparing for the Future
Hospitals, sterilization services, and manufacturers should act now to future-proof their systems:
-
Implement direct part marking using standardised identifiers
-
Adopt electronic tracking systems that link devices to patients and sterilization cycles
-
Use issuing agency-compliant formats (e.g. GS1 or HIBCC) to ensure compatibility with global systems
-
Engage with the TGA's UDI roadmap, and be ready for Class I inclusion
By doing so, they not only support current clinical best practice but will be better positioned when regulations inevitably catch up.
Conclusion
While AS 5369:2023 lays the foundation for safer, more accountable use of reusable surgical instruments, the lack of a corresponding UDI mandate from the TGA leaves a critical gap in Australia’s healthcare safety net.
It’s time for policy to catch up with practice. Aligning TGA regulations with international norms and national clinical standards will not only reduce risk but also reinforce Australia’s commitment to high-quality, patient-centered care.
Check out our FREE resources for simplifying the classification of RMD’s/other Devices into Product Families.
DOWNLOAD YOUR FREE PRODUCT FAMILY MATRIX AND 6-PART VIDEO SERIES
Download your free 'Understanding & Implementing Product Families' eBook
Check out our FREE Product Families Online Course