How does six sigma apply to healthcare and medical practice
 We've all had the experience of sitting in waiting room for what seems and absolute eternity waiting to see a medical professional. Flicking through outdated, dog eared magazines, keeping an eye on the queue, feeling nervous and hoping that it’s your turn next.
We've all had the experience of sitting in waiting room for what seems and absolute eternity waiting to see a medical professional. Flicking through outdated, dog eared magazines, keeping an eye on the queue, feeling nervous and hoping that it’s your turn next.
It’s crazy really, because not only does it create discomfort and dissatisfaction with patients, it also costs the practice significantly in terms of customer satisfaction and higher operating costs.
But why does this happen and, more to the point, how can it be improved?
You don’t know what you don’t know
Well I guess if they knew how to fix it they would fix it. Right? After all it doesn’t make sense to keep people waiting and the practice losing money. It follows then that practice management simply don't know how they can tackle this issue.
That might sound silly, but ever since the industrial revolution, businesses have sought ways to improve their processes and be more efficient.
Six Sigma is a perfect example of this.
Why is it relevant in healthcare?
Six Sigma was in fact created with the idea of improving manufacturing processes. So how does the methodology fit into improving medical practice workflow?
Even though there is a world of difference between manufacturing and running medical practice, in terms of processes they aren't that far apart. Think about it, whether it is cars going down a production line or patients waiting in a line to be seen by a doctor or medical professional, is, from a process point of view, not that dissimilar.
Sure, humans are less predictable than machines and there will always be a certain amount of variation in time and the application of resources when treating people. However I would suggest that it’s probably too simplistic to accept this type of variation as the only reason for the waiting patients. Or is it?
Here is the thing. We just can't be sure because it’s never been measured and analysed. That’s where Six Sigma comes in.
It was designed by Motorola to help improve a failing manufacturing division and has since been implemented in many healthcare settings with much success.
It is a method that seeks to improve the quality of output by identifying the causes of inefficiencies and optimizing the process.
The 5 key phases of Six Sigma
There are 5 key phases captured in the acronym DMAIC:
- Define
- Measure
- Analyse
- Improve
- Control
Define the process, measure its outputs, analyse its outputs, determine improvement opportunities and implement and monitor.
So let’s put this in the context of our waiting room. The waiting room is where the wait manifests. However the cause of the wait lies somewhere else.
Using the principles we would firstly define the process. To do this we can draw a care pathway map.
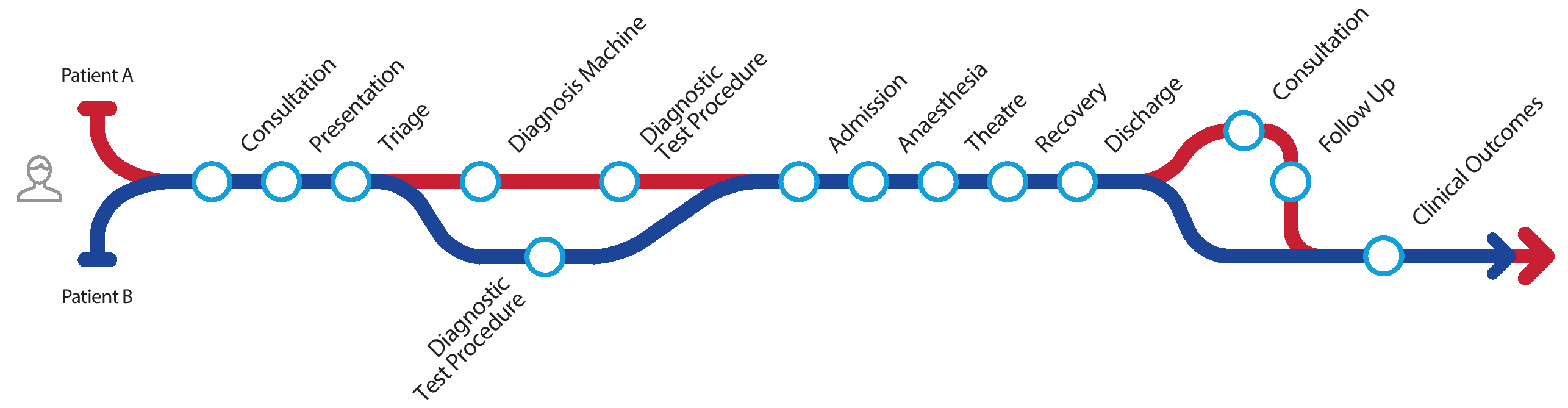
The illustration above shows the patient pathwayincluding possible variations.
Using the second principle we would measure the process. In this case it will be time spent in each location.
Once we have measured, we can move to the 3rd principle Analyse.
The diagram above shows that 2 patients with identical diagnoses have entered the pathway but each have taken slightly different paths.
Once you have accurately tracked the time the patient spent at each stop in the process and identified the variations, you can start to identify bottlenecks and unnecessary delays.
Using the data from the exercise you should be able to identify:
- where unnecessary delays occur
- unnecessary steps taken
- duplication of effort
- bottlenecks
- and understand variations
- and understand the process from a patient’s perspective.
From here you can use the 4th and 5th principles of Six Sigma to improve and control.
Conclusion
Much has been written about the method and its application to healthcare. There are many case studies available on line. But the principles are pretty straightforward. Identify the process to be measured, measure it, analyse it and improve it.
Improving the patient experience and optimising the utilisation of your medical assets are clear benefits of adoption this data driven approach.
A good Patient Administration System or EHR should be able to help you map and identify your processes and calculate the time a patient spends in each area of care. An even better one will provide the data to analyse.