Surgical instrument marking and managing risk.
 Infection control and laser etching medical instruments.
Infection control and laser etching medical instruments.
In my blog What you need to know about Surgical Instrument Direct Part Marking (DPM), I wrote about the benefits of surgical instrument marking. I also touched on some lesser known but important aspects that need to be considered.
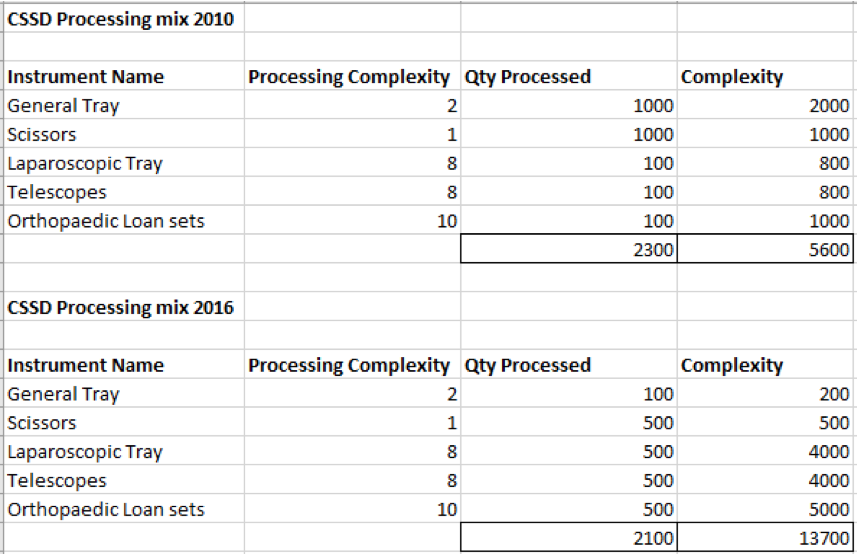
One such aspect is the logistics involved in marking your entire surgical instrument catalog. I used a simple calculation to demonstrate the magnitude of the effort:
Let’s say a reasonable sized facility will have approximately 15,000 surgical instruments. If we mark 6 instruments per hour and multiply that by 8 hours = 48 instruments per day.
Multiply that by 5 days and you have marked 240 instruments a week. Now divide 15,000 by 240 and you will find that it will take 62.5 weeks to mark all your instruments. If you’re a bigger city facility you may have twice or three times that inventory. Do the math on that and you’re talking years!
Just the outcome of that calculation is enough to tempt you to put DPM in the ‘too hard basket’ right?
You may also wonder where you should start and is there any benefit to commence surgical instrument tracking until everything has been etched?
I would like to suggest a different approach. One that can get you started with DPM in a considered and useful way.
I like to call it the ‘risk managed’ approach…
Risk Management and Instrument Etching
So what does risk management have to with etching surgical instruments? Apart from the obvious need to prevent your valuable instruments from going rusty, risk needs to be managed during the implementation phase.
Start where it’s most important. I would suggest begin with instruments that pose the greatest infection risk. This can then be broken into a number of categories and the Spaulding classification system can be used as a start. Spaulding classifies instruments into 3 categories:
- Critical
- Semi-critical
- Non-critical.
Critical instruments are those that enter or penetrate into sterile tissue, body cavities or the bloodstream. So that’s a great place to start. But that still represents many different instruments. Let’s break that down even further.
You could consider the types of procedures that pose the greatest infection risk. An example could be neurosurgery and CJD. So it may make sense to start with surgical instruments that are used in procedures that pose the greatest risk.
Based on this criteria, the instruments that you may choose to etch first could be instruments that are used in:
Neurosurgery, ophthalmic, dental, craniofacial, plastic surgery. Note that I have chosen these as examples because of their close proximity the brain.
How to mark surgical instruments?
 What you physically mark on instruments can have a huge impact on the time it takes to etch your instruments. There are many forms of information you could etch on your instruments, for example:
What you physically mark on instruments can have a huge impact on the time it takes to etch your instruments. There are many forms of information you could etch on your instruments, for example:
- 2D data matrix barcode
- Readable component (in my blog on DPM, I discussed the idea of etching a readable component in case the barcode is unreadable.
- Tray Name
- Instrument Name
- Hospital Name
Obviously you can’t fit all that info on a single instrument. So think about what your objectives are. If you want to assemble instrument sets by scanning, then the 2D data matrix is required. On the other hand, if your objective is infection control and you want to track without scanning 2D barcodes, then you can etch the ID in a readable form and/or the tray name.
The tray name you say for infection control? Well if your objective is infection control you’re going to want to keep your instrument sets unique. To achieve this no data matrix barcodes are needed. By etching a tray name on each instrument – (i.e GEN SET 2, Plastic 1, Dental 5) you can keep your sets together. It also simplifies tray assembly. For example, if you have 50 instruments on a general tray, you simply count 50 instruments marked GEN SET 2.
While that won’t offer you tracking down to the individual instrument level, you need to weigh up cost v benefit. For example, in the event of one instrument on a tray being contaminated, there is a high risk of all instruments being contaminated where they have all been processed together.
Conclusion
You can go to great lengths etching your instruments. However such and exercise would represent a considerable overhead in cost and staff resources. Etching your entire instrument asset will take time. Without an implementation plan, it will be a challenge to get it off the ground. Start with the instruments that pose the greatest risk and decide what level of tracking you really need. A strategy like this will get you up and running safely and in manageable way.