The Untold cost of EMR

Electronic Medical Record systems have now been widely adopted in Australia and around the world. Possibly the most publicised roll out has been in the United States with the government providing significant fiscal incentives under the Meaningful Use program.
In this blog I use the terms EHR and EMR interchangeably.
In the US for example it's common to use EHR (Electronic Health Record) as the term for a patient’s medical record, whereas in Australia, the personal health record system, MyHealth Record is commonly referred to as an EHR. In Australia, the patient record is generally referred to as an EMR (Electronic Medical Record)
Whatever you like to call it, the EMR was looked to as the panacea for the transition to modern efficient delivery of quality healthcare.
However, evidence coming out of the US and Australia demonstrates outcomes quite different to those originally espoused.
An unexpected effect of EHR systems has been the effect it has had on caregivers. Just type "doctor burnout" into google and the return is astonishing. If you follow the links to some of the articles, a very similar theme is present. EHR is burning out our doctors and affecting the delivery and quality of our health care services.
But why?
The implementation of EHR systems has seen a transfer of administrative tasks from medical administrators to doctors and carers.
In her article ‘6 stats on EHR-related physician burnout and 7 tips to combat it’, Julie Spitzer reports that “Half of physicians' average workdays are spent entering data into EHRs and conducting clerical work, while just 27 percent of their workdays are spent with patients.”
A video on the NEJM Catalyst website by Steven Strongwater MD, contains incredibly powerful arguments supporting this effect of EHR on Physicians.
Strongwater uses a graph to highlight the different types of administrative tasks a clinician must do on the EMR, and the time it takes to fulfil those obligations to the EMR after they have seen their patients. The graph demonstrates that a typical day for a physician can start at 4.00am and finish at 9.00pm.
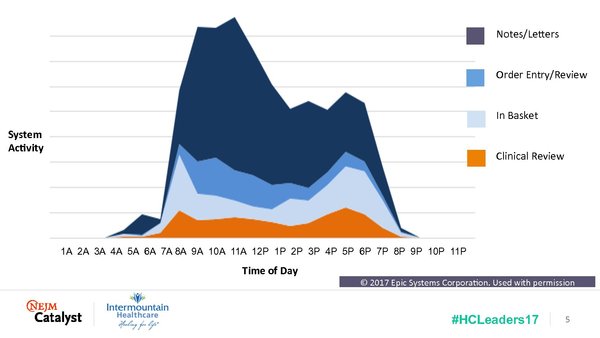
Image Credit: NEJM Catalyst
Strongwater says, “…. we have forced them to make a trade: clicks before care. We have forced them to stare at computer screens and not into the eyes of their patients. We have disrupted that patient-physician bond.”
In their article, To Combat Physician Burnout and Improve Care, Fix the Electronic Health Record, Robert Wachter and Jeff Goldsmith note:
‘After a blizzard of hype surrounding the electronic health record (EHR), health professionals are now in full backlash mode against this complex new tool. They are rightly seen as a major cause of professional burnout among physicians and nurses: Clinicians are spending almost half their professional time typing, clicking, and checking boxes on electronic records.
A common theme across many articles relates to the typical design of EMR’s.
Care givers find them incredibly difficult to use.
Wachter and Goldsmith go onto say, “The electronic systems hospitals have adopted at huge expense are fronted by user interfaces out of the mid-1990s: Windows 95-style screens and dropdown menus, data input by typing and navigation by point and click. These antiquated user interfaces are astonishingly difficult to navigate. Clinical information vital for care decisions is sometimes entombed dozens of clicks beneath the user-facing pages of the patient’s chart.”
Steven Strongwater also makes note in his article, “We look on our cell phones and have such incredible ease of use, and then we look at our electronic medical record screen and we are searching and clicking, and the tools are not quite as sharp, yet, as they need to be.”
An article by Roger Collier titled, Electronic health records contributing to physician burnout, concludes that there are 2 keys to improving the situation with EHR's.
“The first is to build better systems — which may be done by the existing EHR companies or by new tools and apps developed by others,” said Wachter. “The second is to reimagine the work — to think of new ways of providing care that take advantage of the technology without slavishly replicating the old paper-based work and workflow.”
Conclusion
There is considerable evidence coming out of the US and Australia that the widespread adoption of EMR systems is contributing to the burnout of our caregivers.
There seems to be several contributing factors including:
- The transfer of administrative tasks from traditional administrative roles to caregivers.
- The excessive time it takes to complete these administrative obligations
- The complexity of EMR design
- Difficulty of use
- Antiquated interfaces
- Disruption to the patient-doctor bond
Follow this link if you would to learn more about how our EMR alternative – The ScanCARE Digital Document System (DDS), has overcome the issues of Traditional EMR.
You can also download our free Success guide to implementing Digital Medical Records systems